The (A.C.E.s) study shows how much our negative life experiences when we are younger affect us through our lives if we don’t do something about it.
Adverse Childhood Experiences (ACEs) are traumatic or highly stressful events that happen before age 18 and can have long-lasting effects on physical health, mental health, and overall life outcomes.
Here’s a clear breakdown:
- What Counts as an ACE
The original CDC–Kaiser ACE Study identified 10 core categories:
Abuse
- Physical abuse
- Emotional (verbal/psychological) abuse
- Sexual abuse
Neglect
- Physical neglect
- Emotional neglect
Household Dysfunction
- Witnessing domestic violence (especially toward mother figure in the original study)
- Living with someone with substance abuse issues
- Living with someone with mental illness or suicidal behavior
- Parental separation or divorce
- Incarcerated household member
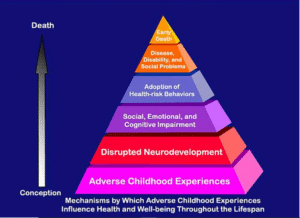
- How ACEs Affect Health
- Stress Response Overload: Chronic stress in childhood can keep the body in “fight–flight–freeze” mode, which over time can damage systems like immunity, digestion, and cardiovascular health.
- Brain Development: Toxic stress can alter brain areas like the amygdala (fear), hippocampus (memory), and prefrontal cortex (decision-making).
- Attachment & Relationships: ACEs can impact trust, self-worth, and ability to form healthy bonds.
- Risk Behaviors: Higher ACE scores correlate with increased smoking, substance use, overeating, unsafe sex, etc.
- Chronic Diseases: Heart disease, diabetes, cancer, COPD, autoimmune disorders have higher incidence in people with higher ACE scores.
- ACE Score
- Each “Yes” to one of the 10 ACE questions = 1 point.
- 0–1 ACEs: lower risk for most negative outcomes
- 4+ ACEs: significantly higher risk for physical, mental, and behavioral health challenges.
(But a high score does NOT mean someone is doomed—protective factors and healing make a huge difference.)
- Protective & Healing Factors
Even with high ACE scores, resilience-building can greatly reduce harm:
- Stable, nurturing relationships (at least one trusted adult)
- Therapy (especially trauma-informed approaches like EMDR, Brainspotting, Somatic Experiencing, CBT)
- Mind–Body Practices (yoga, meditation, breathing, EFT tapping)
- Community connection (friends, spiritual groups, volunteering)
- Healthy lifestyle (exercise, balanced nutrition, sleep hygiene)
- The Hopeful Takeaway
ACEs explain risk—they don’t define destiny.
The brain and body can heal, especially when:
- The trauma is acknowledged
- Skills for emotional regulation are learned
- Supportive environments replace harmful ones
If you’d like, I can make you a high-contrast “ACE Impact & Healing Map” showing causes → effects → resilience strategies so it’s easy to share or use in workshops. That would turn this into a visual one-pager.
Would you like me to create that next?
History, expanded ACE frameworks, neurobiology, lifelong impacts, and recovery science.
- Origins of the ACE Concept
- Research roots: 1995–1997 CDC–Kaiser Permanente ACE Study by Dr. Vincent Felitti & Dr. Robert Anda.
- Purpose: Initially to understand links between childhood trauma and adult health problems.
- Participants: 17,337 adults, mostly middle-class, college-educated, with stable jobs and healthcare access.
- Key finding: ACEs are common and have a dose–response effect — the more ACEs, the higher the risk for poor physical, mental, and social outcomes.
- The Original 10 ACE Categories
Grouped into three domains:
Abuse
- Physical abuse – Being hit, kicked, or physically hurt.
- Emotional abuse – Insults, humiliation, constant criticism.
- Sexual abuse – Sexual contact or exploitation by an older person.
Neglect
- Physical neglect – Not having enough food, clothing, shelter, or medical care.
5. Emotional neglect – Not feeling loved, supported, or emotionally cared for.
Household Dysfunction
6. Mother treated violently – Witnessing domestic violence.
7. Household substance abuse – Living with someone dependent on alcohol/drugs.
8. Household mental illness – Living with someone who is depressed, suicidal, or mentally ill.
9. Parental separation/divorce – Losing a parent through separation, divorce, or abandonment.
10. Incarcerated household member – Parent or close household member in prison/jail.
- Expanded ACE Framework
Since the original study, experts have identified additional ACE-like stressors that also have profound effects on children:
- Community Violence
- Bullying
- Racism or Discrimination
- Poverty / Economic hardship
- Homelessness
- Foster care / Institutionalization
- Natural disasters or war exposure
- Medical trauma (frequent hospitalizations, painful treatments)
- Loss of a loved one (especially sudden or traumatic death)
These are often called Expanded ACEs or Social Determinants of Health ACEs.
- Neurobiology of ACEs
Toxic Stress Response → chronic activation of the body’s HPA axis (Hypothalamic–Pituitary–Adrenal system).
- Amygdala: becomes hyperactive → heightened fear, anxiety, emotional reactivity.
- Hippocampus: can shrink → affecting memory and learning.
- Prefrontal cortex: reduced function → poorer impulse control, planning, and decision-making.
- Epigenetic changes: stress can turn certain genes “on” or “off,” influencing inflammation, immunity, and brain plasticity.
- ACEs & Health Outcomes
The original study and later research found direct links between ACE score and:
- Mental Health: Depression, anxiety, PTSD, substance use disorders, suicide attempts.
- Physical Health: Heart disease, stroke, cancer, diabetes, COPD, chronic pain, autoimmune disease.
- Behavioral Outcomes: Smoking, drug/alcohol abuse, overeating, risky sex, school dropout, unemployment.
- Social Impacts: Relationship instability, incarceration risk, intergenerational trauma.
- The “Dose–Response” Effect
- 0 ACEs: baseline risk
- 1–3 ACEs: moderate increased risk for health/behavioral issues
- 4+ ACEs: sharply higher risk for chronic illness, mental illness, and reduced life expectancy (some studies show up to 20-year reduction on average)
- Intergenerational Effects
- Parents with unresolved ACEs may unintentionally recreate patterns of neglect, abuse, or instability.
- Epigenetic stress markers can be passed down, making children more stress-reactive.
- Healing & Resilience Science
Protective factors can offset ACE harm:
- Stable, loving relationships (even one consistent, caring adult can buffer stress effects)
- Therapeutic interventions:
- EMDR (Eye Movement Desensitization & Reprocessing)
- Brainspotting
- Somatic Experiencing
- Trauma-focused CBT
- Mind–body practices: Yoga, mindfulness, breathwork, EFT tapping.
- Social connection: Friends, mentors, community groups.
- Lifestyle repair: Sleep, nutrition, physical activity.
- Meaning-making: Spirituality, purpose-driven activities.
- ACE Score vs. Resilience Score
- The ACE Score measures risk.
- The Resilience Score measures protective factors (such as supportive adults, safe environments, community ties).
- Together, they give a better picture of someone’s health trajectory than ACE score alone.
If you want, I can now design a professional, one-page “ACEs Deep-Dive Map” that shows:
- Original 10 ACEs
- Expanded ACEs
- Brain & body impacts
- Life outcome risks
- Healing & resilience pathways
1020 Words

Recent Comments